
Table of Contents
REPORT ON DISCUSSING THE PRINCIPLES OF DRUG ADMINISTRATION
Executive summary
This clinical pharmacology report aims to deliver a critical analysis on factors that increase medication errors along with prevention steps that can reduce medication errors. Therefore, this report has focused on the principles of drug administration prescribed by the World health organization. This can be seen from this report. Sometimes the principles of drug administration cannot be maintained and they are worked to increase medication errors in the world. This has larger consequences and this can be stated as the world’s third biggest issues of death. Therefore, the steps of prevention also have been illustrated in this report that emphasized on the storage of medicine, checking during prescribing can helps to the issues of medication errors.
Introduction
Drug administration is a process of giving patients medication to get them over from the disease. Therefore, this is a process that helps patients to get rid of the suffering they have faced. Drug administration should follow some principle that has been set out for the separate kind of disorders and diseases. However, sometime especially after modernisation this has been seen errors on drug administration happen that can be disastrous for a patient’s life. Thus, in this report discussion has been made on the principles of drug administration, consequences of medication errors, factors associated with these errors and steps to prevent errors in drug administration as this aims to demonstrate the importance of principles for administration of drugs.
Factors associated with medication errors
Administration of drugs to the human body consists of different principles that vary from disease to disease. Erdő et al. (2018) have mentioned the route of the drug administration always depending on the problem patients have faced and condition of the patient. Therefore, among all the principles of drug administration vary from disease to disease and patient condition. Some basic principles are there that are prime for each and every health related problem. The basic principles of drug administration are right time, right patient, right drug, right dose, and right route of administration (Yu et al. 2019).
Figure 1: Basic principles of drug administration
(Source: Self developed)
Maintaining the right time for in taking medicines throughout the drug dispensing process is a major principle. Administration of drugs in right times when this is basically needed ensures the patient gets the drug on time when they actually require it. Drugs prescribed in the morning cannot be taken at night unless having permission from a doctor and other health consultants. This has negative implications in the human body (Hilal et al. 2020). Drugs have harmful implications in case of alteration has been seen after ingestion in the body. Drugs may be dangerous in case of alteration; therefore, right patients are only suggested to take right drugs as per their signs and symptoms of disorders after consulting with a healthcare provider as this helps to reduce the risks.
Drugs consist of chemical elements that all are different from one another and used for differential causes or dysfunctionality. Therefore, patients having dysentery ingested headache medicine can be harmful and have negative implications on the body. Thus, right drugs should be taken and prescribed as per the condition of the patient (Brown & Battistella, 2020). Doctor or healthcare provider must have knowledge over the amount of drugs depending on patient’s condition. Therefore, this is one of the important principles of drug administration to take drugs in the right amounts that are required to control the risks of patients. Right route is also one of the principles based on the level of severity and type of medicine that has been taken in home, hospital or any other healthcare giving places. Therefore, this can be stated as one of the principles that have been associated with controlling the risks. For example, drugs such as saline cannot be given through oral route; this must be taken intravenously and helps patients in easy recovery and recover the loss of energy in body (Wu et al. 2020).
In spite of using these principles of proper medication during the entire drug-use process, both the prescribers and patients make mistakes very often. The below discussion made on those factors that lead to medication errors:
Medication errors can be distressful and lead to losses of the patient’s life. Assiri et al. (2018) have stated there are some factors that are associated with medication errors and unsafe practice of doctors and healthcare professionals are associated with these errors in drug administration. The main factors that are associated with medication are discussed below:
Incorrect diagnosis
Incorrect diagnosis of disease is most potential factors associated with medication errors. Cook et al. (2018) have stated diagnosis errors can be happen when faulty test results has been seen, doctors may be unable to understand what is actually in patient’s body according to their symptom. However, doctor by default give him medication for cheat pain due to acidity when he is suffered from heart attack. Therefore, the patient gets medication for acidity can be stated as medication errors due to incorrect diagnosis. On the other hand, this has been reported among total medication errors 68.8% of errors happen due to this reason (Hopkinsmedicine, 2021). However, when patient came to doctor they have to check all their parameters and tests all the probable biomedical and chemical tests to know what actually happen to reduces medication errors.
Confusing handwriting in prescription
Confusing or illegible handwriting of the doctors is also one of the causes of medication errors. Abdi et al. (2018) have mentioned as per their research that poor handwriting of doctors in prescription pushed pharmacists in misconception during honour principles. Therefore, this has been seen from the reports illegible handwriting resulted medication especially errors on the dose of medicine has been seen. For example, in the below prescription this has been seen 1UD demonstrated as 140. This has created confusion to the pharmacists and leads to medication errors.
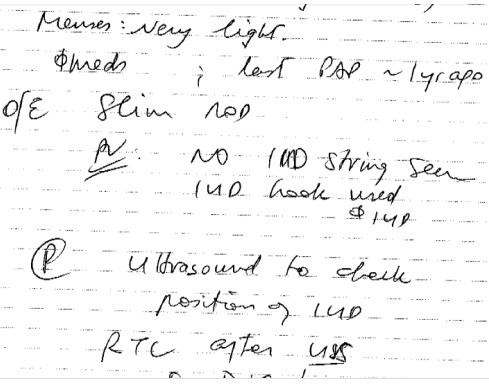
Figure 2: Illegible handwriting in prescription
(Source: Sciencedaily, 2021)
On the other hand, this can be recommended to the doctors while prescribing medicine to patient clearly written the right dose of medicine. In addition, up to 25% of medication errors have been happened due to illegible handwriting of patients (Sciencedaily, 2021).
Poor communication with doctors
Poor communication with doctors also increases medication errors during prescribing medication to the patients. As stated through the research study by Hammoudi et al. (2018), Patients verbally describes their symptoms to the patients can be lack of information or this is not clear to doctors and doctors prescribe medicine according to his understanding can causes medication errors on a serious note. On the other hand, Wheeler et al. (2018) have stated that ineffective communication among health care professional one of the leading cause of medical errors. Due to this cause almost 70% of medication errors has been occurs (Ahrq, 2021). Therefore, this can be recommended to doctors to enhance communication with patients and try to understand what they actually wants to said; this helps to reduces errors ion medication.
Same name and different composition drugs
These types of medication errors mostly associated with the work of pharmacists. This has been seen sometime drugs that have same name; however the molecules of drugs are different. This can be resulted in a severe range of medication errors (Zeng et al. 2022). This has been seen that drug named Zithrimax can be given as alternatives of azithromycin; though, this is not an azithromycin drugs. This is also one of major factor associated with medication errors.
In some time this has been seen that principles of drug administration do not follow in healthcare centre. This led to major consequences and can be life threatening to the life of human beings. Finberg & Guharoy (2021) have stated impacts of medication errors can be seen as a range of mild morbidity to severe mortality. As per the synopsis of this report this has been stated that 7000 deaths per year have occurred due to medication errors. Therefore, this has been seen as a major concern in recent times. From the worldwide health data this has been seen that around 2.8 million patients die due to the drug administration errors (Who, 2021). On the other hand, rates of medication errors vary from one health condition to others.
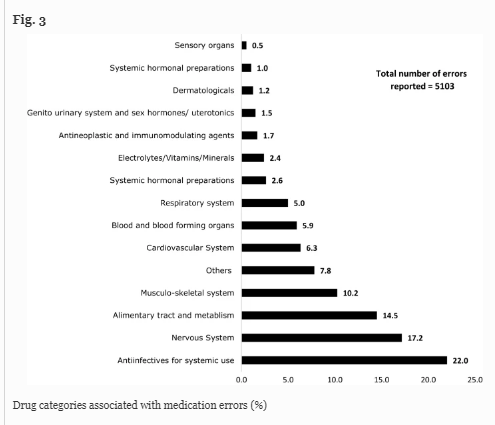
Figure 2: Disease associated with more medication errors
(Source: Thomas et al. 2021)
This graphical representation has been demonstrated that anti infective medicine mostly fall on the category of medication errors as they are complex in nature. Around 22% of medication errors happen with anti infective medicine. Therefore, consequences of medication errors is a major concern and taken as one of the major causes of morbidity. On the contrary, Pshennikov & Angotoeva (2018) have stated medication errors can be defined as the third biggest issues of mortality and morbidity in the entire world. Hence these are major factors of significant cause of morbidity and mortality that lead to patient deaths.
Steps to prevent medication error
Medication errors are one of serious life threatening issues that have been seen from the above section of this report. Thus, it is obvious to be taken for the reduction of these serious issues as early as possible. As stated by Trockel et al. (2018), plans or steps to be taken to prevent medication errors help to improve the health structure of the country and life expectancy of people. The steps to be taken are illustrated below:
- Five basic principles of drug administration should be followed during medication. This has to be ensured by doctors or healthcare providers that they are following the five basic principles of medication helps to reduce incidence of medication errors. This has been described as the use of correct medicine for the correct patient in the correct time and in correct doses through the correct route. Maintaining these principles help to reduces the medication errors and develops the health of people (Billstein-Leber et al. 2018).
- Proper reconciliation of medication procedures or using of proprietary drugs is also important steps that can be maintained during the time of prescription. Proprietary name of medicine also can be known as the brand name that helps people and also the pharmacists in recognition of medicine and reduces medication errors. This actually reduces the incidence of drug alternatives that have negative implications on health. On the other hand, Patel et al. (2019) have stated doctors recommended to follow medication administration records (MAR) to understand what actually the drugs that can be prescribed to patients depending on their condition.
- This is also very important to recheck what is written in prescription by doctors. On the other hand, doctors should double check or even triple check to rectify issues due to illegible handwriting of doctors. This has been seen that rechecking of prescription helps to reduces issues due to illegible hand watering and medication errors in dose and drugs. On the other hand, Giuliano (2018) have stated pharmacists also recommended transcribing the doctor prescription correctly and reducing medication errors. Double and triple check on the prescription reduces medication errors from doctors and pharmacists also.
- Right process of drug amounting by physicians is also one of the steps that reduce medication errors or errors in drug administration. Therefore, this has been stated that the steps have to be done through the right amounting procedures and doctors are recommended to put a “zero” when places a decimal amount before the dose amount, for example, doctors prescribe to patient that a medicine should be taken in amount of .25 mg; however, patients do not understand this and take this on amount of 25 mg. Therefore, doctors should put a”0” before a dose of drugs. This helps to reduce medication errors in drug doses (Giuliano, 2018).
- Medication errors also can happen from spoilage of medicine due to long term storage. Therefore, this can be an excellent step to keep medicine through proper storage. Therefore, it can be stated that education should be kept refrigerated when there is a need for refrigeration in a specific medicine. On the other hand, in some cases multidisc of a vial is needed and this should be kept in refrigeration to avoid spoilage in education and reduce errors in administration.
- This is a fundamental responsibility of pharmacists and people to check the level of drugs to know the further information on drugs. This checking process helps to understand manufacturing, expiry dates along with other legal information and certification of drugs. This has been seen some time pharmacists sell the product over the expiry dates and this causes discomfort and disability in people (Giuliano, 2018). Therefore, rechecking everything before selling a drug can be a useful strep to be followed for reduction of medication errors
- Being alerted on popular names is also a step to be taken for prevention of medication errors. There are some popular medicine brand names that people can easily believe. Taking this as an advantage, imitation of the brand can be done easily. This led to discomfort of people who are ingesting copy medication and medication errors can also happen with this. For example, Johnson is one of the popular medicine brands; therefore, this can be imitated any time and causes medication errors and this especially impacts on child skin and health. Johnson is one of the popular medicine brands for children.
- Dispensing the right drug also can be done through the process of using clear abbreviation and a proper handwriting. This has been seen that pharmacists has some key roles in drugs prescribing, dispensing and administration. Therefore, medical practitioner who has the right to dispense medicine should use clear abbreviation and proper handwriting. This also has been seen from that clear abbreviation reduces the incidence of medication errors and helps people to protect their health. On the other hand, this also can be stated to rectify the problem of medication errors through the process of proper diagnosis. Doctors should use each and every possible measure to understand the spectrum of the disease along with consequences and prescribing medicine according to this. For example, patient having symptoms of heart disease must take care of patients through prescribing them each and every biomedical and chemical test that can be associated with symptoms of patients. This helps to reduce medication errors and helps people to rectify themselves from their condition (Giuliano, 2018).
Conclusion
Hence, this can be concluded from the entire discussion on this report that principles of drug administration should be maintained by healthcare centres and professionals to overcome the consequences of faulty drug administration in people’s life. This also has been stated that medication has five basic principles for administration of drugs that can be maintained during the time of prescribing drugs to the patients. This can be concluded that factors associated with medication errors can have a mild to severe range on people’s body and they are suffering from discomfort and disability in body. This has been seen that factors associated with medication errors can be associated from doctors, pharmacists and patients itself also. Thus, there is an illustrated discussion based on the steps that can be preventing the medication errors. Therefore, this can be stated that errors not only prevented in administration rather the prevention of the incidence starts from the root level. This have been concluded from the report that distorts should check their prescription during the time prescribing drugs to the patients. Storage of drugs is measures that should be keep in mind when someone deals with drugs that helps in reduction of spoilage and reduces medication errors. Thus, after reviewing this report this can be recommended to establish drug administration principles when someone deals with drugs.
References
Abdi, M., Piri, S., Mohammadian, R., Asadi, M., & Khademi, E. (2018). Factors associated with medication errors in the psychiatric ward of Razi Hospital in Tabriz: Perspectives of nurses. Preventive Care in Nursing and Midwifery Journal, 8(2), 1-8.
Ahrq (2021), Improving Patient Safety Through Provider Communication Strategy Enhancements
Billstein-Leber, M., Carrillo, C. J. D., Cassano, A. T., Moline, K., & Robertson, J. J. (2018). ASHP guidelines on preventing medication errors in hospitals. American Journal of Health-System Pharmacy, 75(19), 1493-1517., R. S., Sekhri, S., Bhimanadham, N. N., Imran, S., & Hossain, S. (2019). A review on strategies to manage physician burnout. Cureus, 11(6).
Brown, P., & Battistella, M. (2020). Principles of drug dosing in sustained low efficiency dialysis (SLED) and review of antimicrobial dosing literature. Pharmacy, 8(1), 33.
Cook, D. A., Sherbino, J., & Durning, S. J. (2018). Management reasoning: beyond the diagnosis. Jama, 319(22), 2267-2268.
Cook, G. A., Shebl, N. A., Mahmoud, M. A., Aloudah, N., Grant, E., Aljadhey, H., & Sheikh, A. (2018). What is the epidemiology of medication errors, error-related adverse events and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ open, 8(5), e019101.
Erdő, F., Bors, L. A., Farkas, D., Bajza, Á., & Gizurarson, S. (2018). Evaluation of intranasal delivery route of drug administration for brain targeting. Brain Research Bulletin, 143, 155-170.
Finberg, R. W., & Guharoy, R. (2021). Basic principles of drug delivery and dosing. In Clinical Use of Anti-infective Agents (pp. 5-21). Springer, Cham.
Giuliano, K. K. (2018). Intravenous smart pumps: usability issues, intravenous medication administration error, and patient safety. Critical Care Nursing Clinics, 30(2), 215-224.
Hammoudi, B. M., Ismaile, S., & Abu Yahya, O. (2018). Factors associated with medication administration errors and why nurses fail to report them. Scandinavian journal of caring sciences, 32(3), 1038-1046.
Hilal, T., Gonzalez-Velez, M., & Prasad, V. (2020). Limitations in clinical trials leading to anticancer drug approvals by the US Food and Drug Administration. JAMA internal medicine, 180(8), 1108-1115.
Hopkinsmedicine (2021), Diagnostic Errors More Common, Costly And Harmful Than Treatment Mistakes
Karimian, Z., Kheirandish, M., Javidnikou, N., Asghari, G., Ahmadizar, F., & Dinarvand, R. (2018). Medication errors associated with adverse drug reactions in Iran (2015-2017): A P-method approach. International journal of health policy and management, 7(12), 1090.
Moriarty, F., Bennett, K., & Fahey, T. (2019). Fixed-dose combination antihypertensives and risk of medication errors. Heart, 105(3), 204-209.
Pshennikov, D. S., & Angotoeva, I. B. (2018). Principles of drug therapy for acute bacterial rhinosinusitis: from evidence-based medicine to practice. IP Pavlov Russian Medical Biological Herald, 26(1), 106-116.
Sciencedaily (2021), Computerized Doctors’ Orders Reduce Medication Errors
Thomas, B., Pallivalapila, A., El Kassem, W., Al Hail, M., Paudyal, V., McLay, J., … & Stewart, D. (2021). Investigating the incidence, nature, severity and potential causality of medication errors in hospital settings in Qatar. International journal of clinical pharmacy, 43(1), 77-84.
Trockel, M., Bohman, B., Lesure, E., Hamidi, M. S., Welle, D., Roberts, L., & Shanafelt, T. (2018). A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Academic Psychiatry, 42(1), 11-24.
Wheeler, A. J., Scahill, S., Hopcroft, D., & Stapleton, H. (2018). Reducing medication errors at transitions of care is everyone’s business. Australian prescriber, 41(3), 73.
Who (2021), WHO calls for urgent action to reduce patient harm in healthcare
Wu, D., Pusuluri, A., Vogus, D., Krishnan, V., Shields IV, C. W., Kim, J., … & Mitragotri, S. (2020). Design principles of drug combinations for chemotherapy. Journal of Controlled Release, 323, 36-46.
Yu, J., Petrie, I. D., Levy, R. H., & Ragueneau-Majlessi, I. (2019). Mechanisms and clinical significance of pharmacokinetic-based drug-drug interactions with drugs approved by the US Food and Drug Administration in 2017. Drug Metabolism and Disposition, 47(2), 135-144.
Zeng, Z., Yao, Y., Liu, Z., & Sun, M. (2022). A deep-learning system bridging molecule structure and biomedical text with comprehension comparable to human professionals. Nature communications, 13(1), 1-11.
